Quinidine as a cause of sudden death.
Circulation. 1956; 14: 757-765
Generation of 3D functional microvascular networks with human mesenchymal stem cells in microfluidic systems.
Integr. Biol. (Camb.). 2014; 6: 555-563
A vascularized and perfused organ-on-a-chip platform for large-scale drug screening applications.
Lab Chip. 2017; 17: 511-520
Long-term maintenance of a microfluidic 3D human liver sinusoid.
Biotechnol. Bioeng. 2016; 113: 241-246
Design and fabrication of a liver-on-a-chip platform for convenient, highly efficient, and safe in situ perfusion culture of 3D hepatic spheroids.
Lab Chip. 2018; 18: 2547-2562
Rapid wire casting: a multimaterial microphysiological platform enabled by rapid casting of elastic microwires.
Adv. Healthc. Mater. 2019; 81970019
Instrumented cardiac microphysiological devices via multimaterial three-dimensional printing.
Nat. Mater. 2017; 16: 303-308
A complex human gut microbiome cultured in an anaerobic intestine-on-a-chip.
Nat. Biomed. Eng. 2019; 3: 520-531
Mature induced-pluripotent-stem-cell-derived human podocytes reconstitute kidney glomerular-capillary-wall function on a chip.
Nat. Biomed. Eng. 2017; 1: 0069
Characterization of a microfluidic in vitro model of the blood-brain barrier (muBBB).
Lab Chip. 2012; 12: 1784-1792
Microfluidic 3D bone tissue model for high-throughput evaluation of wound-healing and infection-preventing biomaterials.
Biomaterials. 2012; 33: 999-1006
Drawing inspiration from developmental biology for cardiac tissue engineers.
Adv. Biol. (Weinh.). 2021; 5e2000190
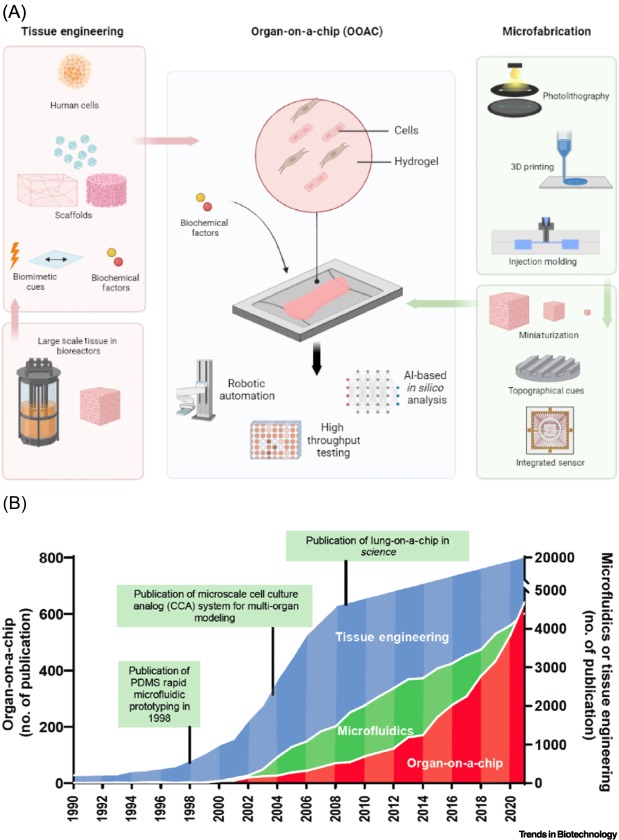
Rapid prototyping of microfluidic systems in poly(dimethylsiloxane).
Anal. Chem. 1998; 70: 4974-4984
The design and fabrication of three-chamber microscale cell culture analog devices with integrated dissolved oxygen sensors.
Biotechnol. Prog. 2004; 20: 338-345
Reconstituting organ-level lung functions on a chip.
Science. 2010; 328: 1662-1668
Muscle LIM protein force-sensing mediates sarcomeric biomechanical signaling in human familial hypertrophic cardiomyopathy.
Circulation. 2022; 145: 1238-1253
A platform for generation of chamber-specific cardiac tissues and disease modeling.
Cell. 2019; 176: 913-927
Extracellular matrix as an inductive scaffold for functional tissue reconstruction.
Transl. Res. 2014; 163: 268-285
Extracellular matrix bioscaffolds in tissue remodeling and morphogenesis.
Dev. Dyn. 2016; 245: 351-360
Engineering microenvironment for human cardiac tissue assembly in heart-on-a-chip platform.
Matrix Biol. 2020; 85–86: 189-204
Skin-on-a-chip model simulating inflammation, edema and drug-based treatment.
Sci. Rep. 2016; 6: 37471
Development of a primary human small intestine-on-a-chip using biopsy-derived organoids.
Sci. Rep. 2018; 8: 2871
Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors.
Cell. 2006; 126: 663-676
Induction of pluripotent stem cells from adult human fibroblasts by defined factors.
Cell. 2007; 131: 861-872
Heart disease. Titin mutations in iPS cells define sarcomere insufficiency as a cause of dilated cardiomyopathy.
Science. 2015; 349: 982-986
Modeling the mitochondrial cardiomyopathy of Barth syndrome with induced pluripotent stem cell and heart-on-chip technologies.
Nat. Med. 2014; 20: 616-623
Evidence for cardiomyocyte renewal in humans.
Science. 2009; 324: 98-102
Towards chamber specific heart-on-a-chip for drug testing applications.
Adv. Drug Deliv. Rev. 2020; 165-166: 60-76
Advanced maturation of human cardiac tissue grown from pluripotent stem cells.
Nature. 2018; 556: 239-243
Structural and functional maturation of cardiomyocytes derived from human pluripotent stem cells.
Stem Cells Dev. 2013; 22: 1991-2002
Advanced physiological maturation of iPSC-derived human cardiomyocytes using an algorithm-directed optimization of defined media components.
bioRxiv. 2022; ()
Abstract 291: In vitro matured human embryonic stem cell-derived cardiomyocytes form grafts with enhanced structure and improved electromechanical integration in injured hearts.
Circ. Res. 2020; 127: A291
Development of a functional glomerulus at the organ level on a chip to mimic hypertensive nephropathy.
Sci. Rep. 2016; 6: 31771
Human gut-on-a-chip inhabited by microbial flora that experiences intestinal peristalsis-like motions and flow.
Lab Chip. 2012; 12: 2165-2174
Biowire model of interstitial and focal cardiac fibrosis.
ACS Central Sci. 2019; 5: 1146-1158
Intersection of stem cell biology and engineering towards next generation in vitro models of human fibrosis.
Front Bioeng. Biotechnol. 2022; 101005051
Macrophages of diverse phenotypes drive vascularization of engineered tissues.
Sci. Adv. 2020; 6eaay6391
Vasculature-on-a-chip platform with innate immunity enables identification of angiopoietin-1 derived peptide as a therapeutic for SARS-CoV-2 induced inflammation.
Lab Chip. 2022; 22: 1171-1186
Tunable electroconductive decellularized extracellular matrix hydrogels for engineering human cardiac microphysiological systems.
Biomaterials. 2021; 272120764
Anisotropic engineered heart tissue made from laser-cut decellularized myocardium.
Sci. Rep. 2016; 6: 32068
3D culture of HepaRG cells in GelMa and its application to bioprinting of a multicellular hepatic model.
Biomaterials. 2021; 269120611
Fabrication of modular hyaluronan-PEG hydrogels to support 3D cultures of hepatocytes in a perfused liver-on-a-chip device.
Biofabrication. 2019; 11015013
Recapitulating pancreatic tumor microenvironment through synergistic use of patient organoids and organ-on-a-chip vasculature.
Adv. Funct. Mater. 2020; 302000545
Three-dimensional in vitro cell culture models in drug discovery and drug repositioning.
Front. Pharmacol. 2018; 9: 6
A well plate-based multiplexed platform for incorporation of organoids into an organ-on-a-chip system with a perfusable vasculature.
Nat. Protoc. 2021; 16: 2158-2189
PDMS microfluidics: a mini review.
J. Appl. Polym. Sci. 2020; 137: 48958
Quantitative analysis of molecular absorption into PDMS microfluidic channels.
Ann. Biomed. Eng. 2012; 40: 1862-1873
Progress in three-dimensional bioprinting.
MRS Bull. 2017; 42: 557-562
Microfabricated tuneable and transferable porous PDMS membranes for organs-on-chips.
Sci. Rep. 2018; 8: 13524
Soft lithography.
Annu. Rev. Mater. Sci. 1998; 28: 153-184
Polymer microfluidics: simple, low-cost fabrication process bridging academic lab research to commercialized production.
Micromachines. 2016; 7: 225
Advances in microfluidic devices made from thermoplastics used in cell biology and analyses.
Biomicrofluidics. 2017; 11051502
A multimaterial microphysiological platform enabled by rapid casting of elastic microwires.
Adv. Healthc. Mater. 2019; 8e1801187
E-FLOAT: extractable floating liquid gel-based organ-on-a-chip for airway tissue modeling under airflow.
Adv. Mater. Technol. 2021; 62100828
Fabrication of polymer microfluidics: an overview.
Polymers (Basel). 2022; 14: 2028
Fibrotic microtissue array to predict anti-fibrosis drug efficacy.
Nat. Commun. 2018; 9: 2066
Multimodal characterization of cardiac organoids using integrations of pressure-sensitive transistor arrays with three-dimensional liquid metal electrodes.
Nano Lett. 2022; 22: 7892-7901
Intracellular recording of human cardiac action potentials on market-available multielectrode array platforms.
Front Bioeng. Biotechnol. 2020; 8: 66
High-speed mechano-active multielectrode array for investigating rapid stretch effects on cardiac tissue.
Nat. Commun. 2019; 10: 834
Massive rearrangements of cellular microRNA signatures are key drivers of hepatocyte dedifferentiation.
Hepatology. 2016; 64: 1743-1756
Characterization of primary human hepatocytes, HepG2 cells, and HepaRG cells at the mRNA level and CYP activity in response to inducers and their predictivity for the detection of human hepatotoxins.
Cell Biol. Toxicol. 2012; 28: 69-87
Augmentation of EB-directed hepatocyte-specific function via collagen sandwich and SNAP.
Biotechnol. Prog. 2008; 24: 1132-1141
Regulation of cell morphology and cytochrome P450 expression in human hepatocytes by extracellular matrix and cell-cell interactions.
Cell Tissue Res. 2001; 306: 85-99
P-glycoprotein expression, localization, and function in sandwich-cultured primary rat and human hepatocytes: relevance to the hepatobiliary disposition of a model opioid peptide.
Pharm. Res. 2004; 21: 1294-1302
Microscale culture of human liver cells for drug development.
Nat. Biotechnol. 2008; 26: 120-126
Layered patterning of hepatocytes in co-culture systems using microfabricated stencils.
Biotechniques. 2010; 48: 47-52
Spheroid-based three-dimensional liver-on-a-chip to investigate hepatocyte-hepatic stellate cell interactions and flow effects.
Lab Chip. 2013; 13: 3529-3537
A microfluidic 3D hepatocyte chip for drug toxicity testing.
Lab Chip. 2009; 9: 2026-2035
Liver sinusoid on a chip: Long-term layered co-culture of primary rat hepatocytes and endothelial cells in microfluidic platforms.
Biotechnol. Bioeng. 2015; 112: 2571-2582
A high-throughput microfluidic microphysiological system (PREDICT-96) to recapitulate hepatocyte function in dynamic, re-circulating flow conditions.
Lab Chip. 2019; 19: 1556-1566
A micro cell culture analog (microCCA) with 3-D hydrogel culture of multiple cell lines to assess metabolism-dependent cytotoxicity of anti-cancer drugs.
Lab Chip. 2009; 9: 1385-1394
Liver-on-a-chip platform to study anticancer effect of statin and its metabolites.
Biochem. Eng. J. 2021; 165107831
Multi-tissue interactions in an integrated three-tissue organ-on-a-chip platform.
Sci. Rep. 2017; 7: 8837
HiPSC-derived multi-organoids-on-chip system for safety assessment of antidepressant drugs.
Lab Chip. 2021; 21: 571-581
Three-dimensional perfused human in vitro model of non-alcoholic fatty liver disease.
World J. Gastroenterol. 2017; 23: 204-215
A reductionist metastasis-on-a-chip platform for in vitro tumor progression modeling and drug screening.
Biotechnol. Bioeng. 2016; 113: 2020-2032
Three-dimensional human liver-chip emulating premetastatic niche formation by breast cancer-derived extracellular vesicles.
ACS Nano. 2020; 14: 14971-14988
Prevascularization of cardiac patch on the omentum improves its therapeutic outcome.
Proc. Natl. Acad. Sci. U. S. A. 2009; 106: 14990-14995
Pluripotent stem cell-derived cardiac tissue patch with advanced structure and function.
Biomaterials. 2011; 32: 9180-9187
Scaffold-free human cardiac tissue patch created from embryonic stem cells.
Tissue Eng. Part A. 2009; 15: 1211-1222
High-density seeding of myocyte cells for cardiac tissue engineering.
Biotechnol. Bioeng. 2003; 82: 403-414
Functional assembly of engineered myocardium by electrical stimulation of cardiac myocytes cultured on scaffolds.
Proc. Natl. Acad. Sci. U. S. A. 2004; 101: 18129-18134
Three-dimensional engineered heart tissue from neonatal rat cardiac myocytes.
Biotechnol. Bioeng. 2000; 68: 106-114
A microfabricated platform to measure and manipulate the mechanics of engineered cardiac microtissues.
Tissue Eng. Part A. 2012; 18: 910-919
Optimizing engineered heart tissue for therapeutic applications as surrogate heart muscle.
Circulation. 2006; 114: I72-I78
Pre-treatment of synthetic elastomeric scaffolds by cardiac fibroblasts improves engineered heart tissue.
J. Biomed. Mater. Res. A. 2007; 86: 713-724
Human cardiac fibrosis-on-a-chip model recapitulates disease hallmarks and can serve as a platform for drug testing.
Biomaterials. 2020; 233119741
Engineered 3D cardiac fibrotic tissue to study fibrotic remodeling.
Adv. Healthc. Mater. 2017; 6201601434
Design and fabrication of biological wires for cardiac fibrosis disease modeling.
in: Coulombe K.L.K. Black Iii L.D. Cardiac Tissue Engineering: Methods and Protocols. Springer, 2022: 175-190
Tissue engineering of a differentiated cardiac muscle construct.
Circ. Res. 2002; 90: 223-230
Engineered heart tissue grafts improve systolic and diastolic function in infarcted rat hearts.
Nat. Med. 2006; 12: 452-458
Physiological calcium combined with electrical pacing accelerates maturation of human engineered heart tissue.
Stem Cell Rep. 2022; 17: 2037-2049
Machine learning of human pluripotent stem cell-derived engineered cardiac tissue contractility for automated drug classification.
Stem Cell Rep. 2017; 9: 1560-1572
Cardiopatch platform enables maturation and scale-up of human pluripotent stem cell-derived engineered heart tissues.
Nat. Commun. 2017; 8: 1825
I-wire heart-on-a-chip I: three-dimensional cardiac tissue constructs for physiology and pharmacology.
Acta Biomater. 2017; 48: 68-78
Miniaturized iPS-cell-derived cardiac muscles for physiologically relevant drug response analyses.
Sci. Rep. 2016; 6: 24726
Human engineered heart tissue as a versatile tool in basic research and preclinical toxicology.
PLoS One. 2011; 6e26397
Human iPSC-based cardiac microphysiological system for drug screening applications.
Sci. Rep. 2015; 5: 8883
Functional microvascularization of human myocardium in vitro.
Cell Rep. Methods. 2022; 2100280
Shortening velocity causes myosin isoform shift in human engineered heart tissues.
Circ. Res. 2021; 128: 281-283
Biowire: a platform for maturation of human pluripotent stem cell-derived cardiomyocytes.
Nat. Methods. 2013; 10: 781-787
Ensembles of engineered cardiac tissues for physiological and pharmacological study: heart on a chip.
Lab Chip. 2011; 11: 4165-4173
Microfluidic heart on a chip for higher throughput pharmacological studies.
Lab Chip. 2013; 13: 3599-3608
Mussel-inspired 3D fiber scaffolds for heart-on-a-chip toxicity studies of engineered nanomaterials.
Anal. Bioanal. Chem. 2018; 410: 6141-6154
NHLBI family blood pressure program: methodology and recruitment in the HyperGEN network. Hypertension genetic epidemiology network.
Ann. Epidemiol. 2000; 10: 389-400
An organ-on-a-chip model for pre-clinical drug evaluation in progressive non-genetic cardiomyopathy.
J. Mol. Cell. Cardiol. 2021; 160: 97-110
Mapping signalling perturbations in myocardial fibrosis via the integrative phosphoproteomic profiling of tissue from diverse sources.
Nat. Biomed. Eng. 2020; 4: 889-900
Contractile deficits in engineered cardiac microtissues as a result of MYBPC3 deficiency and mechanical overload.
Nat. Biomed. Eng. 2018; 2: 955-967
Synergistic engineering: organoids meet organs-on-a-chip.
Cell Stem Cell. 2017; 21: 297-300
In vitro metabolic zonation through oxygen gradient on a chip.
Sci. Rep. 2019; 9: 13557
Metabolic patterning on a chip – towards in vitro liver zonation of primary rat and human hepatocytes.
Sci. Rep. 2018; 8: 8951
DLL4 and VCAM1 enhance the emergence of T cell-competent hematopoietic progenitors from human pluripotent stem cells.
Sci. Adv. 2022; 8eabn5522
A multi-organ chip with matured tissue niches linked by vascular flow.
Nat. Biomed. Eng. 2022; 6: 351-371
Programming cellular alignment in engineered cardiac tissue via bioprinting anisotropic organ building blocks.
Adv. Mater. 2022; 342200217
Rapid 3D bioprinting of decellularized extracellular matrix with regionally varied mechanical properties and biomimetic microarchitecture.
Biomaterials. 2018; 185: 310-321
FDA Modernization Act of 2021.
117th Congress. 2021–2022
Regenerative medicine: the emergence of an industry.
J. R. Soc. Interface. 2010; 7: S771-S775
Tissue engineering: the design and fabrication of living replacement devices for surgical reconstruction and transplantation.
Lancet. 1999; 354: st32-st34
Soft Lithography.
Angew. Chem. Int. Ed. 1998; 37: 550-575
Biomimetic approach to cardiac tissue engineering: oxygen carriers and channeled scaffolds.
Tissue Eng. 2006; 12: 2077-2091
Mathematical model of oxygen distribution in engineered cardiac tissue with parallel channel array perfused with culture medium containing oxygen carriers.
Am. J. Physiol. Heart Circ. Physiol. 2005; 288: H1278-H1289
Organoid model in idiopathic pulmonary fibrosis.
Int. J. Stem Cells. 2021; 14: 1-8
3D bioprinting of mechanically tuned bioinks derived from cardiac decellularized extracellular matrix.
Acta Biomater. 2021; 119: 75-88
Soft lithography based on photolithography and two-photon polymerization.
Microfluid. Nanofluid. 2018; 22: 97
- SEO Powered Content & PR Distribution. Get Amplified Today.
- Platoblockchain. Web3 Metaverse Intelligence. Knowledge Amplified. Access Here.
- Source: https://www.cell.com/trends/biotechnology/fulltext/S0167-7799(22)00346-8?rss=yes
- 1
- 2021
- 3d
- 7
- a
- academic
- accelerates
- Act
- Action
- activity
- Adult
- advanced
- analysis
- and
- Application
- applications
- approach
- Array
- Assembly
- assessment
- authors
- Automated
- barrier
- based
- Basel
- basic
- biology
- Biomaterials
- Black
- Blocks
- blood
- Blood Pressure
- BONE
- bridging
- Building
- bull
- carriers
- Cause
- causes
- Cells
- central
- Chamber
- Channel
- channels
- chip
- classification
- combined
- complex
- components
- conditions
- Congress
- construct
- Convenient
- created
- Culture
- D.C.
- Death
- Derived
- Design
- Detection
- Dev
- Development
- developmental
- device
- Devices
- differentiated
- discovery
- Disease
- distribution
- diverse
- drive
- drivers
- drug
- drug development
- drug discovery
- drug testing
- Drugs
- dynamic
- ed
- effect
- effects
- efficient
- emergence
- enabled
- enables
- Engineering
- Engineers
- enhanced
- evaluation
- Experiences
- factors
- family
- floating
- flow
- form
- formation
- from
- function
- functional
- functions
- generation
- grown
- Heart
- higher
- highly
- HTTPS
- human
- Humans
- Hypertension
- Identification
- immunity
- improve
- improved
- improves
- in
- industry
- inflammation
- innate
- Inspiration
- integrated
- integration
- integrations
- interactions
- Interface
- investigate
- Key
- kidney
- lab
- large-scale
- layered
- learning
- Level
- lines
- linked
- Liquid
- List
- Liver
- living
- Localization
- long-term
- made
- maintenance
- Matrix
- measure
- mechanical
- mechanics
- Media
- medicine
- medium
- Meet
- metal
- Methodology
- methods
- Microbiome
- model
- modeling
- models
- modernization
- modular
- MOL
- molecular
- mRNA
- multiple
- nano
- Nanomaterials
- network
- networks
- next
- ONE
- optimization
- overview
- Oxygen
- Parallel
- part
- Patch
- patient
- platform
- Platforms
- plato
- Plato Data Intelligence
- PlatoData
- polymer
- predict
- pressure
- primary
- process
- Production
- profiling
- Program
- progression
- progressive
- properties
- Protein
- protocols
- prototyping
- rapid
- RAT
- rearrangements
- recording
- recruitment
- relevance
- relevant
- research
- response
- result
- review
- safe
- Safety
- SARS-CoV-2
- scale-up
- SCI
- screening
- sensors
- serve
- shift
- Signatures
- Simple
- small
- Snap
- Sources
- specific
- Stem
- stem cells
- structure
- studies
- Study
- sudden
- support
- surgical
- synthetic
- system
- Systems
- Technologies
- Testing
- The
- their
- Therapeutic
- three-dimensional
- Through
- throughput
- tissues
- to
- tool
- towards
- treatment
- under
- union
- use
- VeloCity
- versatile
- via
- W
- Wire
- X
- zephyrnet